Elizabeth Siegel Watkins
The Johns Hopkins University Press
Baltimore, Maryland
2007
351 pages
According to the Art:
The book is about estrogen from the 1890s until the early 2000s. Covered is the evolution of estrogen use, and how over time it affected feminism, pharmaceutical promotion, patient advocacy, patient information, conceptions of menopause, evidence standards, cultural shifts, and media influences.
Synopsis:
Elizabeth Siegel Watkins reports on the use of estrogen alone and in combination with progestin for women during menopause and after menopause from the 1890s until the book was published in 2007. She concentrates on the sixty years between 1942 and 2002. The event Watkins uses to mark 1942 as an important moment is the U.S. Food and Drug Administration (FDA) approval for the estrogen product Premarin as hormone replacement therapy (HRT) in women with menopause symptoms. The event she uses to mark 2002 is the release Women’s Health Initiative (WHI) findings that showed estrogen is not the “elixir of life” that many thought it was then.
Watkins builds her story off the trajectory of estrogen use during this sixty-year period, which spans two peaks followed by two crashes. The estrogens for HRT first crested in the early 1970s before its use dropped dramatically in 1975 on uterine cancer fears. Estrogen use began to rise in the early 1980s on regained confidence from combined use with progestin to reduce uterine cancer risk and from hopes that bone loss could be prevented and even reversed. This resurrection continued through the 1990s as estrogen use during and after menopause became “associated with reduced risk of colon cancer, prevention of tooth loss, lower incidence of osteoarthritis, increase in bone mass, reduced risk of Alzheimer’s disease, and lower rates of death from all causes.” (p. 241)
Based on surveys of prescribers and prescription data during this time, Watkins concludes that “physicians who saw menopausal women as patients were…enthusiastic prescribers of HRT.” (p. 244) They remained enthusiastic, making Premarin the most prescribed pharmaceutical product through much of the 1990s and until 2002 when the WHI trial was stopped three years early because it showed that HRT failed to produce the expected benefits, and even worse.
Women who took the estrogen–progestin pills, as compared with those in the control group who took placebo pills, increased their risk of breast cancer by 26 percent (relative risk of 1.26), coronary heart disease by 29 percent (1.29), stroke by 41 percent (1.41), and pulmonary embolism (blood clot) by 213 percent (2.13).
p. 271

Accessed at WHI.org
The investigators advised clinicians based on these results, that HRT “should not be initiated or continued for the primary prevention of coronary heart disease.” (p. 271) Watkins quotes an editorial from the Journal of the American Medical Association that went further in saying that the trial “provides an important health answer for generations of health postmenopausal women to come—do not use estrogen / progestin to prevent chronic disease.” (p. 273) HRT prescriptions plummeted.
These clinical inputs into the trajectory of estrogen are just the bare bones of estrogen history. Watkins fills in the story:
The story of estrogen is woven from several strands: blind faith in the ability of science and technology to solve a broad range of health and social problems, social and cultural stigmatization of aging, shifting meanings and interpretations of femininity and female identity, and the pitfalls of medical hubris in the twentieth century. (p. 1)
p. 1
Watkins weaves these strands into the story of estrogen, which she tells in a chronological fashion, often as the subjects of individual chapters. Some include: the implications of rising feminism; pharmaceutical company promotional activities; the roles of patient advocacy organizations; FDA requirements for patient information about prescription drugs; generational differences in views of menopause; evolving research methods and evidence standards; and cultural shifts and mainstream media influences.
Analysis:
The trajectory Watkins covers is long enough—one hundred and seventeen years—for her to show how the history of estrogen reflects secular trends through the period, and how estrogen generated trends itself. As she unfurls the history of estrogen use she reveals some notable history of Biomedicine at the same time, in particular, the discovery and development of hormones, the rise of medicalization, the growth of women’s health and patient advocacy groups, the advancement of patient education, and the evolution of clinical research standards.
Watkins links the discovery of estrogen in the late nineteenth and early twentieth centuries to the broader scientific work on secretions from organs that affect other parts of the body. In addition to estrogen secretion from ovaries were insulin secretion from the pancreas and thyroxine secretion from thyroid glands. These secretions became known as “hormones.” They were eventually crystallized and used in humans to good effect (“organotherapy”). These developments gave the medical profession confidence that it could address (“medicalize”) “‘normal’ life-course events, such as childbirth, menopause, and aging.” (p. 3) Watkins notes that this confidence extended to the public as it acceded to the “cultural authority and prestige of both the practice and the practitioners of science.” (p. 19) In the case of estrogen, the public’s confidence would not be rewarded in the long run, as would be the case also for a variety of promising treatments through the twentieth century and into the twenty-first.
The concept of medicalization plays a big part of the estrogen story Watkins tells. Menopause was considered a normal phase of women’s lives through the millennia preceding medical means to affect it. To biomedical practitioners, institutions, and product manufacturers, once there became pharmacological interventions to address signs, symptoms, and consequences of menopause, it became a medical problem for them to solve. “Menopause is a pathologic rather than physiologic phenomenon…requiring active intervention,” Watkins quotes a prominent physician and journal editor of the American Journal of Obstetrics and Gynecology as saying in 1962. (p. 47) The problem eventually extended from menopause to “also the long-term prevention of debility and disease associated with aging.” (p. 49) By the 1970s, “the consensus of opinion among American and Western European physicians…indicated strong approval of the more comprehensive application of estrogen in older women’s health care.” (p. 49) They put their prescriptions where their mouths were; Premarin was among the top five prescription drugs in the U.S. in 1975.
Accessed from nwhn.org
The movement to medicalize menopause did not go unopposed. Watkins describes how the feminist movement of the 1960s and 1970s collided with the biomedical movement to medicalize menopause. She points to some of the feminist groups that took on issues related to women’s health (e.g., National Women’s Health Network), and how hormonal treatments, particularly those used for menopause, became a galvanizing issue for these groups. The feminist objection was “to the characterization of menopause as a disease.” (p. 188) But, Watkins is quick to point out that the feminist groups were not against Science or Biomedicine research efforts to learn more about menopause. “What they opposed was the incursion of the pharmaceutical industry into medical research and practice, with the assumption that research must result in a commercial medication for doctors to prescribe to patients.” (p. 188).
These and other differences resulted in a feminist model of menopause and aging that was distinguishable from the medical model. The feminist model placed more emphasis on the psychosocial aspects of menopause than on physiological elements, and also on managing menopause and aging through “diet, exercise, and spiritual, emotional, and intellectual fulfillment.” (p. 190) Watkins wondered which model female obstetricians and gynecologists would follow. She found survey data showing that “women physicians prescribed HRT more often than their male counterparts did,” and that “patients seen by female physicians were more than five times as likely to begin ERT.” Female physicians practice what they preach as they also “used HRT themselves at a much higher rate than did the general public.” (p. 245)
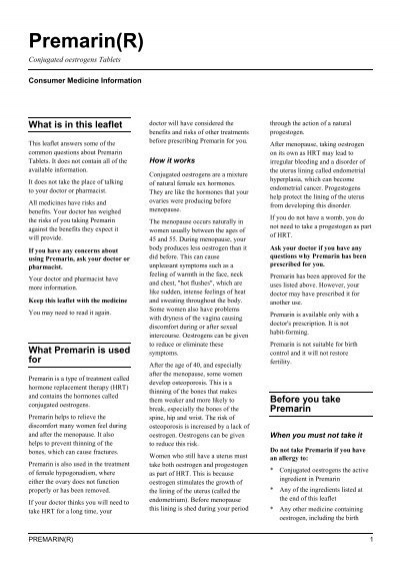
Although patient information leaflets accompanied all prescriptions for oral contraceptives beginning in 1970, Watkins argues that the association of uterine cancer with estrogen use in menopause was the event that led eventually to this becoming a requirement for all prescription drugs. She also recognizes that the calls for getting more information to patients corresponded “with a general loss of confidence in medicine in the 1970s, as doctors and hospitals faced challenges to their political influence, economic power, and cultural authority from the women’s movement, the consumers’ movement, and the patients’ rights movement. (p. 133) These patient rights’ advocates, and a generally supportive FDA, had to overcome objections from pharmaceutical manufacturers and health care providers over concerns about government intrusions into the practice of medicine and the ability of patients to comprehend and use the information. But, they did.
Watkins also considers how the change in evidentiary standards affected the trajectory of estrogen use for menopause. Fueling the two peaks in estrogen use for menopause were personal anecdotes, case studies, and epidemiological analyses, which do not involve randomization of subjects. Watkins groups these methods as “observational” studies and notes how they became “deficient by modern standards.” (p. 50) The rising standards of research methods and expectations of evidence-based medical practice led to testing the effectiveness of estrogen for menopause with randomized controlled trials (RCTs). WHI was the most notable result.
Watkins closes showing how the trajectory she followed ends where it began by quoting a 2005 NIH consensus statement following the results of WHI, which starts with, “Menopause is a natural process that occurs in women’s lives as part of normal aging,” and ends with, “Menopause is ‘medicalized’ in contemporary U.S. society. There is a great need to develop and disseminate information that emphasizes menopause as a normal, healthy phase of women’s lives and promotes its demedicalization.” (pp. 283–284)
The book ends there, but the story continues. Subsequent analyses of the published trials and publication of new studies added complexity to the benefit – risk assessments that led to the precipitous drop in HRT. The complexity involves different results seen based on study designs, ages of women in the studies, and the number of years women were followed among other factors. These differences suggest that certain subgroups of women could benefit from HRT. As a result, a growing sentiment is seeping back into the mainstream media advocating for more liberal use of it. Watkins will have more to work with if she takes up her story where she left off.
Also:
A version of this review is posted here at the NYU Literature, Art and Medicine Database.